Intracytoplasmic Sperm Injection (ICSI)
It is postulated that some cases of male infertility may be explained by the presence of chromosomal abnormalities, DNA damage or a combination of both. Intracytoplasmic Sperm Injection (ICSI) as Treatment for male–factor infertility has been introduced worldwide in the past few years in many laboratories using Assisted Reproduction Techniques. Intracytoplasmic Sperm Injection (ICSI) has been successful in cases of extreme oligoasthenozoospermia in achieving pregnancies via In–Vitro Fertilization (IVF) with the lowest imaginable sperm counts. For inclusive representing and understanding of the above–mentioned complexities of andrological infertility, it is essential to reveal the essence of the fertilization process in two dimensions: natural and assisted ones. The special emphasis is given to the representation of the basics of both fertilization processes with a special emphasis on their peculiarities, including their comparison with the special focus on differences.
Introduction
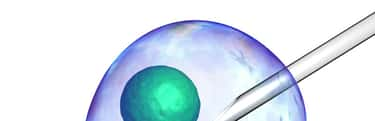
Intracytoplasmic Sperm Injection (ICSI) is the most efficient variant of micromanipulation–assisted fertilization used in Assisted Reproduction Technology (ART) to overcome various types of male factor infertility, whereby a single ‘top–quality’ spermatozoon is accurately selected, aspirated into a microinjection needle and injected to the oocyte cytoplasm. High success rates have been reported for the use of Intracytoplasmic Sperm Injection (ICSI) in alleviating essentially andrological infertility.
Generally representing the whole process, in Intracytoplasmic Sperm Injection (ICSI) sperm chromatin is introduced into the oocyte together with the acrosome, a structure that does not enter the oocyte during normal fertilization. The development of this technique is mainly linked to application in assisted reproduction for which it enables fertilization with defective spermatozoa that would not otherwise be able to penetrate an oocyte by their proper means. Because Intracytoplasmic Sperm Injection (ICSI) by–passes many phases of the natural fertilization process, it offers an extremely interesting model for the study of basic mechanisms underlying fertilization. Oocyte activation is a series of events triggered by the fertilizing spermatozoon and necessary for the beginning of the embryonic development. The morphological normality of a spermatozoon is considered to be an important factor in relation to its ability to fertilize an oocyte. Only one condition had a strongly negative influence on the result of Intracytoplasmic Sperm Injection (ICSI): where an immotile (presumably dead) spermatozoon was injected into the oocyte. Thus the only ultimate criterion for successful Intracytoplasmic Sperm Injection (ICSI) is the presence of at least one living spermatozoon per oocyte in the pellet of the treated semen sample used for micro–injection. This is particularly true for oocyte activation, whose mechanism needs to be revisited in light of the current Intracytoplasmic Sperm Injection (ICSI) research. The massive application of Intracytoplasmic Sperm Injection (ICSI) in Infertility Treatment also represents a huge laboratory in which the impact of different genetic and epigenetic anomalies of the male gamete on fertilization and embryonic development can be studied [Tesarik and Mendoza 1999].
1. Inclusive representation of the overview of the process of natural fertilization. The essential peculiarities of the process of natural fertilization: the concepts and conclusions represented in the study “Sperm chromatin remodeling after Intracytoplasmic Sperm Injection differs from that of In Vitro Fertilization” written by Ajduk A., Yamauchi Y., Ward A.M.
Reproduction is mediated by specialized cells, the male (spermatozoon) and the female (oocyte) gametes, whose chromosome and DNA content has been reduced to half (haploid) compared with diploid somatic cells. This reduction is mediated by two successive meiotic divisions, of which only the first is preceded by a DNA synthetic phase, and is realized during gametogenesis (spermatogenesis and oogenesis) within the testis and the ovary. Spermatozoa reach competence for fertilization and fuse with the oocytes in the female reproductive tract. First, spermatozoa undergo a process called capacitation (from “capacity to fertilize oocytes”), during which numerous molecular changes in the sperm take place, resulting in sperm becoming competent to undergo the acrosome reaction. During acrosome reaction the membrane surrounding the acrosome fuses with the plasma membrane of the sperm, releasing acrosome contents and rendering sperm capable of penetrating zona pellucida. The result of acrosome reaction is that the equatorial region of the sperm membrane is exposed and fuses with the oolemma, facilitating introduction of the sperm nucleus into the oocyte. Once in the ooplasm, the sperm nucleus undergoes several structural changes, known as chromatin remodeling. One component of global remodeling is the assembly of histones; others involve chromatin maturation, positioning of nucleosomes, and addition of other DNA–binding proteins [Ajduk et al., 2006]. During fertilization, spermatozoon and an oocyte unite to create a diploid zygote, whose future successive mitotic divisions give rise to all cells of an embryo [Tesarik and Mendoza 1999].
2. Inclusive representation of the overview of the process of Assisted Fertilization. The essential peculiarities of the process of Assisted Fertilization: the concepts and conclusions represented in the study “Sperm chromatin remodeling after Intracytoplasmic Sperm Injection differs from that of In Vitro Fertilization” written by Ajduk A., Yamauchi Y., Ward A.M.
When fertilization does not occur in a natural way, various approaches of Assisted Fertilization can be used by fertility experts. The most popular are In Vitro Fertilization (IVF) and Intracytoplasmic Sperm Injection (ICSI) [Ajduk et al., 2006]. Intracytoplasmic Sperm Injection (ICSI) involves the direct injection of a single spermatozoon into a metaphase II arrested oocyte, thus bypassing many of the steps normally present in gamete interactions, both during in–vivo and In–Vitro Fertilization. These include the sperm acrosome reaction, sperm–zona binding and penetration, and sperm–oolemma binding and fusion [Hewitson et al., 2000]. In In Vitro Fertilization (IVF), capacitation and acrosome reaction are achieved through maintaining specific culture conditions during gamete co–incubation. The sperm fuses with the oocyte in a similar manner, as it takes place during fertilization in vivo [Ajduk et al., 2006]. In Intracytoplasmic Sperm Injection (ICSI), capacitation, acrosome reaction, and membrane fusion are bypassed. Sperm chromatin enters ooplasm together with the perinuclear material, acrosome, and cell membrane [Ajduk et al., 2006]. Although these components eventually disintegrate inside the oocyte, it was suggested that they might interfere with sperm chromatin remodeling [Hewitson et al., 1996; Sutovsky et al., 2003; Ramalho–Santos et al., 2000]. Healthy babies were born with Intracytoplasmic Sperm Injection (ICSI), and the technique is considered successful. However, existing reports on a higher incidence of chromosome aberrations [In’t Veld et al., 1997; Macas et al., 2001], lower developmental potentials [Shoukir et al., 1998; Tesarik and Mendoza 1999; Dumoulin et al., 2000; Bhattacharya et al., 2001], and abnormal calcium oscillations [Tesarik and Mendoza 1999] in embryos produced with Intracytoplasmic Sperm Injection (ICSI) indicate that further evaluations on Intracytoplasmic Sperm Injection (ICSI) effects are needed [Ajduk et al., 2006]. Consequently, what is essential to emphasize is that Assisted Reproductive Treatments, Intracytoplasmic Sperm Injection (ICSI) in particular, bypass natural barriers that might normally prevent fertilization with abnormal spermatozoa. The incidence of de novo chromosomal abnormalities has been reported to be higher in Intracytoplasmic Sperm Injection (ICSI) conceptions compared with natural conceptions [Lam et al., 2001; Bonduelle et al., 2002; Gjerris et al., 2008].
Conclusion
Since its inclusive implementation in clinical practice, Intracytoplasmic Sperm Injection (ICSI) has challenged a number of established reproductive paradigms. High success rates have been reported for the use of Intracytoplasmic Sperm Injection (ICSI) in alleviating essentially andrological infertility. Considering the fact that it bypasses many steps normally completed during traditional fertilization, the success of Intracytoplasmic Sperm Injection (ICSI) provokes questions as to what is necessary and/or sufficient for productive gamete interactions. The morphological normality of a spermatozoon is considered to be an important factor in relation to its ability to fertilize an oocyte. Only one condition had a strongly negative influence on the result of Intracytoplasmic Sperm Injection (ICSI): where an immotile (presumably dead) spermatozoon was injected into the oocyte. Thus, the only ultimate criterion for successful Intracytoplasmic Sperm Injection (ICSI) is the presence of at least one living spermatozoon per oocyte in the pellet of the treated semen sample used for micro–injection.
In conclusion, it should be indicated that for the comprehensive understanding of Assisted Fertilization the comparative analysis of the various Assisted Reproductive Technology’s methods should be done. The special emphasis should be given to dissection of the peculiar choreography of fertilization by Intracytoplasmic Sperm Injection (ICSI) and In Vitro Fertilization (IVF) at the subcellular level, revealing the obvious abnormalities, asynchronous elements and hidden complexities of both methods for establishing the most accurate paradigms of further investigations and for prevention of negative consequences of Artificial Insemination methods on ultrastructural level. Notably, the unusual handling of sperm components not present inside the oocyte during conventional in–vitro fertilization, as well as the possible implications for the first embryonic cell cycle, should be investigated. Given the ethical dilemmas involved, information from a clinically relevant model is needed. Such a model could help expand the information and of impaired reproductive quality.
References
[1] Ajduk A., Yamauchi Y., Ward A.M. Sperm chromatin remodeling after intracytoplasmic sperm injection differs from that of in vitro fertilization. Biology of Reproduction, 2006; 75(3): 442–451.
[2] Bhattacharya S., Hamilton M.P., Shaaban M., Khalaf Y., Seddler M., Ghobara T., Braude P., Kennedy R., Rutherford A., Hartshorne G., Templeton A. Conventional in–vitro fertilization versus intracytoplasmic sperm injection for the treatment of non-male-factor infertility: a randomised controlled trial. Lancet, 2001; 357: 2075–2079.
[3] Bonduelle M., Aytoz A., Van Assche E. et al. Incidence of chromosomal aberrations in children born after assisted reproduction through intracytoplasmic sperm injection. Hum. Reprod., 1998a; 13: 781–782.
[4] Bonduelle M., Joris H., Hofmans K. et al. Mental development of 201 ICSI children at 2 years of age. Lancet, 1998b; 351: 1553.
[5] Bonduelle M., Van Assche E., Joris H., Keymolen K., Devroey P., Van Steirteghem A., Liebaers I. Prenatal testing in ICSI pregnancies: incidence of chromosomal anomalies in 1586 karyotypes and relation to sperm parameters. Hum. Reprod., 2002; 17: 2600–2614.
[6] Bourgain C., Nagy Z.P., De Zutter H. et al. Ultrastructure of gametes after intracytoplasmic sperm injection. Hum. Reprod., 1998; 13 (Suppl. 1): 107–116.
[7] Breitbart H., Spungin B. The biochemistry of the acrosome reaction. Mol. Hum. Reprod., 1997; 3: 195–202.
[8] Dumoulin J.C., Coonen E., Bras M., van Wissen L.C., Ignoul–Vanvuchelen R., Bergers–Jansen J.M., Derhaag J.G., Geraedts J.P., Evers J.L. Comparison of in–vitro development of embryos originating from either conventional in–vitro fertilization or intracytoplasmic sperm injection. Hum. Reprod., 2000; 15:402–409.
[9] Gjerris A.C., Loft A., Pinborg A., Christiansen M., Tabor A. Prenatal testing among women pregnant after assisted reproductive techniques in Denmark 1995–2000: a national cohort study. Hum. Reprod., 2008; 23: 1545–1552.
[10] Gotte M., von Mollard G.F. A new beat for the SNARE drum. Trends Cell Biol., 1998; 8: 215–218.
[11] Hanson P.I., Heuser J.E., Jahn, R. Neurotransmitter release ø four years of SNARE complexes. Curr. Opin. Neurobiol., 1997; 7: 310–315.
[12] Hewitson L.C., Simerly C.R., Tengowski M.W., Sutovsky P., Navara C.S., Haavisto A.J., Schatten G. Microtubule and chromatin configurations during rhesus intracytoplasmic sperm injection: successes and failures. Biol, Reprod., 1996; 55: 271–280.
[13] Hewitson L., Simerly C., Dominko T. et al. Cellular and molecular events after in vitro fertilization and intracytoplasmic sperm injection. Theriogenology, 2000; 53: 95–104.
[14] In’t Veld P., Brandenburg H., Verhoeff A. et al. Sex chromosomal abnormalities and intracytoplasmic sperm injection. Lancet, 1995; 346(8977): 773.
[15] Lam R., Ma S., Robinson W.P., Chan T., Yuen B.H. Cytogenetic investigation of fetuses and infants conceived through intracytoplasmic sperm injection. Fertil. Steril., 2001; 76: 1272–1275.
[16] Macas E., Imthurn B., Keller P.J. Increased incidence of numerical chromosome abnormalities in spermatozoa injected into human oocytes by ICSI. Hum. Reprod., 2001; 16: 115–120.
[17] Ramalho–Santos J., Moreno R.D., Sutovsky P. et al. SNAREs in mammalian sperm: possible implications for fertilization. Dev. Biol., 2000; 223: 54–69.
[18] Ramalho–Santos J., Sutovsky P., Simerly C., Oko R., Wessel G.M., Hewitson L., Schatten G. ICSI choreography: fate of sperm structures after monospermic rhesus ICSI and first cell cycle implications. Hum. Reprod., 2000; 15: 2610–2620.
[19] Rothman J.E. Mechanisms of intracellular protein transport. Nature, 1994; 372: 55–63
[20] Shoukir Y., Chardonnens D., Campana A., Sakkas D. Blastocyst development from supernumerary embryos after intracytoplasmic sperm injection: a paternal influence? Hum. Reprod., 1998; 13: 1632–1637.
[21] Sutovsky P., Manandhar G., Wu A., Oko R. Interactions of sperm perinuclear theca with the oocyte: implications for oocyte activation, anti-polyspermy defense, and assisted reproduction. Microsc. Res. Tech., 2003; 61: 362–378.
[22] Tesarik J., Mendoza C. In vitro fertilization by intracytoplasmic sperm injection. Bioessays, 1999; 21: 791–801.
[23] Wassarman P.M. Mammalian fertilization: molecular aspects of gamete adhesion, exocytosis, and fusion. Cell, 1999; 96: 175–183.